This is an old revision of this page, as edited by Hordaland (talk | contribs) at 17:39, 16 August 2010 (punctuation, readability, wikilink). The present address (URL) is a permanent link to this revision, which may differ significantly from the current revision.
Revision as of 17:39, 16 August 2010 by Hordaland (talk | contribs) (punctuation, readability, wikilink)(diff) ← Previous revision | Latest revision (diff) | Newer revision → (diff)| The neutrality of this article's introduction is disputed. Relevant discussion may be found on the talk page. Please do not remove this message until conditions to do so are met. (August 2010) (Learn how and when to remove this message) |
| It has been suggested that this article be merged into Depression (mood). (Discuss) Proposed since August 2010. |

Depression, one of the most commonly diagnosed psychiatric disorders, is thought to occur primarily due to dysregulation of neurotransmitters in the brain such as serotonin and dopamine.
The diagnosis of depression is being made in increasing numbers, in various segments of the population, most notably college students. In a study by Hofstra University in New York, the records of 3,256 college students seeking counseling at an on-campus clinic between 1997 and 2009 were examined. Students diagnosed with depression increased from 34 to 41 percent; those on psychiatric medications increased from eleven to 24 percent.
There are many psychiatric and medical conditions that may mimic some or all of the symptoms of depression, or may occur comorbid to depression. A disorder either psychiatric or medical that shares symptoms and characteristics of another disorder, and may be the true cause of the presenting symptoms is known as a differential diagnosis.
Many ostensibly psychiatric disorders such as depression are diagnosed by allied health professionals with little or no medical training such as psychotherapists. Individuals lacking medical training have been shown in general to be deficient in diagnosing medical conditions masquerading as psychiatric illness.
Study findings suggest that non-medical mental health care providers may be at increased risk of not recognizing masked medical illnesses in their patients. (Grace GD, Christensen RC 2007)
In cases where a diagnosis is made by a medical professional, adequate screening out of differential diagnoses is often not conducted.
Many diagnoses are made on the basis of presenting symptoms without proper consideration of the underlying cause. Potential differential diagnoses are often never taken into consideration or are arbitrarily dismissed without benefit of medical testing, and in many cases without a medical history being taken into consideration.
A plea is made for careful medical evaluation of psychiatric patients. (Hall RC et al. 1978).
Misdiagnosis or missed diagnoses may lead to lack of treatment or ineffective and potentially harmful treatment which may worsen the underlying causitive disorder.
Often those with a psychiatric condition also have a comorbid medical disorder which, if undiagnosed and untreated, compounds the treatment of the primary disorder.
In a case of misdiagnosed depression recounted in Newsweek, a writer received treatment for depression for years; during the last 10 years of her depression the symptoms worsened resulting in multiple suicide attempts and psychiatric hospitalizations. When an MRI finally was performed it showed the presence of a tumor. She was however told by a neurologist that it was benign. After a worsening of symptoms, upon the second opinion of another neurologist, the tumor was removed. After the surgery she no longer suffered from depression.
Autoimmune disorders
- Celiac disease; is an autoimmune disorder in which the body is unable to digest gluten, found in various grains such as rye and barley. Current research has shown it is neuropsychiatric symptoms may manifest without the gastrointestinal symptoms.
However, more recent studies have emphasized that a wider spectrum of neurologic syndromes may be the presenting extraintestinal manifestation of gluten sensitivity with or without intestinal pathology.
- Lupus: Systemic lupus erythematosus (SLE), is a chronic autoimmune connective tissue disease that can affect any part of the body. Lupus can cause or worsen depression.
Bacterial-viral-parasitic infection

- Lyme disease; is a bacterial infection caused by Borrelia burgdorferi, a spirochete bacterium transmitted by the Deer tick (ixodes scapulari). Lyme disease is one of a group of diseases which have earned the name the "great imitator" for their propensity to mimic the symptoms of a wide variety of medical and neuropsychiatric disorders.
- Syphilis; the prevalence of which is on the rise, is another of the "great imitators", which if left untreated can progress to neurosyphilis and affect the brain, can present with solely neuropsychiatric symptoms. This case emphasises that neurosyphilis still has to be considered in the differential diagnosis within the context of psychiatric conditions and diseases. Owing to current epidemiological data and difficulties in diagnosing syphilis, routine screening tests in the psychiatric field are necessary. (Friedrich F. et al. 2009)
- Neurocysticercosis (NCC): is an infection of the brain or spinal cord caused by the larval stage of the pork tapeworm, Taenia solium. NCC is the most common helminthic (parasitic worm) infestation of the central nervous system worldwide. Humans develop cysticercosis when they ingest eggs of the pork tapeworm via contact with contaminated fecal matter or eating undercooked infected pork . While cysticercosis is endemic in Latin America, it is an emerging disease with increased prevalence in the United States. The rate of depression in those with neurocysticercosis is higher than in the general population.
- Toxoplasmosis; is an infection caused by Toxoplasma gondii an intracellular protozoan parasite. Humans can be infected in 3 different ways: ingestion of tissue cysts, ingestion of oocysts, or in utero infection with tachyzoites. One of the prime methods for transmission to humans is contact with the feces of the host species, the domesticated cat. Toxoplasma gondii infects approximately 30% of the world's human population, but causes overt clinical symptoms in only a small segment of those infected. Exposure to Toxoplasma gondii (seropositivity) without developing Toxoplasmosis has been proven to alter various characteristics of human beahvior as well as being a causative factor in some cases of depression.
- West Nile virus (WNV); which can cause encephalitis has been reported to be a causal factor in developing depression in 31% of those infected in a study conducted in Houston, Texas and reported to the Center for Disease Control (CDC). The primary vectors for disease transmission to humans are various species of mosquito.
Blood disorders
- Anemia: is a decrease in normal number of red blood cells (RBCs) or less than the normal quantity of hemoglobin in the blood. Depressive symptoms are associated with anemia in a general population of older persons living in the community (Onder G et al. 2005).
Chronic fatigue syndrome
Between 1 and 4 million Americans are believed to have from Chronic Fatigue Syndrome (CFS), yet only 50% have consulted a physician for CFS symptoms CFS. In addition of those with CFS symptoms have an undiagnosed medical or psychiatric disorder such as diabetes, thyroid disease or substance abuse. CFS, at one time considered to be psychosomatic in nature is now considered to be a valid medical condition in which early diagnosis and treatment can aid in alleviating or completely resolving symptoms.While frequently misdiagnosed as depression,differences have been noted in rate of cerebral blood flow.
CFS is underdiagnosed in more than 80% of the people who have it; at the same time, it is often misdiagnosed as depression. (Griffith JP, Zarrouf FA.,2008)
Dietary disorders
- Fructose malabsorption and lactose intolerance; deficient fructose transport by the duodenum, or by the deficiency of the enzyme, lactase in the mucosal lining, respectively. As a result of this malabsorption the saccharides reach the colon and are digested by bacteria which convert them to short chain fatty acids, CO2, and H2. Approximately 50% of those afflicted exhibit the physical signs of irritable bowel syndrome
- Fructose malabsorption may play a role in the development of depressed mood. Fructose malabsorption should be considered in patients with symptoms of major depression....(Ledochowski M, et al. 1998)
- Fructose and sorbitol reduced diet in subjects with fructose malabsorption does not only reduce gastrointestinal symptoms but also improves mood and early signs of depression (Ledochowski M, et al. 2000).
Endocrine system disorders
Dysregulation of the endocrine system may present with various neuropsychiatric symptoms, irregularities in the hypothalamic-pituitary- adrenal (HPA) axis and the hypothalamic-pituitary-thyroid (HPT) axis have been shown in patients with primary depression (Musselman DL, Nemeroff CB. 1996)
| HPT and HPA axes abnormalities observed in patients with depression (Musselman DL, Nemeroff CB. 1996) | ||||
|
HPT axes irregularities:
HPA axes irregularities:
|
Adrenal gland
- Addison's disease: also known as chronic adrenal insufficiency, hypocortisolism, and hypocorticism) is a rare endocrine disorder wherein the adrenal glands, located above the kidneys, produce insufficient steroid hormones (glucocorticoids and often mineralocorticoids). Addison's disease presenting with psychiatric features in the early stage has the tendency to be overlooked and misdiagnosed.
Thyroid and parathyroid glands

- Graves' disease:an autoimmune disease where the thyroid is overactive, resulting in hyperthyroidism and thyrotoxicosis.
- Hashimoto's thyroiditis: also known chronic lymphocytic thyroiditis is an autoimmune disease in which the thyroid gland is gradually destroyed by a variety of cell and antibody mediated immune processes. Hashimoto's thyroiditis is associated with thyroid peroxidase and thyroglobulin autoantibodies
- Hypothyroidism
- Hyperthyroidism
- Hypoparathyroidism; can affect calcium homeostasis, supplementation of which has completely resolved cases of depression in which Hypoparathyroidism is the sole causative factor.
Pituitary tumors
Tumors of the pituitary gland are fairly common in the general population with estimates ranging as high as 25%. Most tumors are considered to be benign and are often an incidental finding discovered during autopsy or as of neuroimaging in which case they are dubbed "incidentalomas". Even in benign cases, pituitary tumors can affect cognitive, behavioral and emotional changes. Pituitary microadenomas are smaller than 10 mm in diameter and are generally considered benign, yet the presence of a microadenoma has been positively identified as a risk factor for suicide.
... "patients with pituitary disease were diagnosed and treated for depression and showed little response to the treatment for depression".
Pancreas
- Hypoglycemia: an overproduction of insulin causes reduced blood levels of glucose. In one study of patients recovering from acute lung injury in intensive care, those patients who developed hypoglycemia while hospitalized showed an increased rate of depression.
Neurological
In addition to pituitary tumors, tumors in various locations in the central nervous system may cause depressive symptoms and be misdiagnosed as depression.
Post concussion syndrome
Post-concussion syndrome (PCS), is a set of symptoms that a person may experience for weeks, months, or occasionally years after a concussion with a prevalence rate of 38–80% in Mild traumatic brain injuries, it may also occur in moderate and severe cases of traumatic brain injury. A diagnosis may be made when symptoms resulting from concussion, depending on criteria, last for more than three to six months after the injury, in which case it is termed Persistent postconcussive syndrome (PPCS). In a study of the prevalence of post concussion syndrome symptoms in patients with depression utilizing the British Columbia Postconcussion Symptom Inventory: Approximately 9 out of 10 patients with depression met liberal self-report criteria for a postconcussion syndrome and more than 5 out of 10 met conservative criteria for the diagnosis These self reported rates were significantly higher than those obtained in a scheduled clinical interview. Normal controls have exhibeted symptoms of PCS as well as those seeking psychological services. There is considerable debate over the diagnosis of PCS in part because of the medico-legal and thus monetary ramifications of receiving the diagnosis.(Iverson GL. 2006)
Pseudobulbar affect
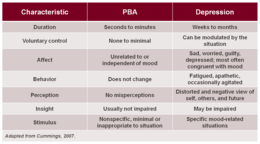
Pseudobulbar affect (PBA) is an affective disinhibition syndrome that is largely unrecognized in clinical settings and thus often untreated due to ignorance of the clinical manifestations of the disorder, it may be misdiagnosed as depression. It often occurs secondary to various neurodegenerative diseases such as Amyotrophic lateral sclerosis, and also can result from head trauma. PBA is characterized by involuntary and inappropriate outbursts of laughter and/or crying. PBA has a high prevalence rate with estimates of 1.5 - 2 million cases in the United States alone
Neurotoxicity
Various compounds have been shown to have neurotoxic effects many of which have been implicated as having a causal relationship in the development of depression.
Cigarette smoking
There is a proven correlation between cigarette smoking and depression. Studies have suggested that smoking cigarettes may have a direct causal effect on the development of depression and that smoking cessation may have a therapeutic effect on ameliorating the symptoms of depression in smokers diagnosed with depressive disorders. There have been various studies done showing a positive link between smoking, suicidal ideation and suicide attempts. In a study conducted among nurses, those smoking between 1-24 cigarettes per day had twice the suicide risk; 25 cigarettes or more, 4 times the suicide risk, than those who had never smoked. In a study of 300,000 male U.S. Army soldiers, a defintive link between suicide and smoking was observed with those smoking over a pack a day having twice the suicide rate as non-smokers.
| Link Between Smoking Depression and Suicide | ||||
|
Current daily smoking, but not past smoking, predicted the subsequent occurrence of suicidal thoughts or attempt It would seem unwise, nevertheless, to rule out the possibility that smoking might be among the antecedent factors associated with the development of depression (Murphy JM et al. 2003). Abstinence from cigarettes for prolonged periods may be associated with a decrease in depressive symptomatology (Lembke A et al. 2007) The stress induction model of smoking suggests, however, that smoking causes stress and concomitant negative affect (Aronson KR. et al. 2008). |
Medication
Various medications have been suspected of a having a causal relation in the development of depression this has been classified as organic mood syndrome. Some classes of medication such as those used to treat hypertension, have been recognized for decades as having a definitive relationship with the development of depression.
Monitoring for the development of depressive symptoms for those taking medications which have shown a relationship with depression is often indicated, as well as the necessity of factoring in the use of such medications in the diagnostic process.
- Topical Tretinoin (Retin-A); derived from Vitamin A and used for various medical conditions such as in topical solutions used to treat acne vulgaris. Although applied externally to the skin may enter the bloodstream and cross the blood brain barrier where it may have neurotoxic effects.
- Interferons; proteins produced by the human body, three types have been identified alpha, beta and gamma. Synthetic versions are utilized in various medications used to treat different medical conditions such as the use of interferon-alpha in cancer treatment and hepatitis C treatment. All three classes of interferons may cause depression and suicidal ideation.
Neuropsychiatric
Bipolar disorder
- Bipolar disorder is frequently misdiagnosed as major depression, and is thus treated with antidepressants alone which is not only not efficacious it is often contraindicated as it may exacerbate hypomania, mania, or cycling between moods.J Clin Psychiatry. 2005 Nov;66(11):1432-40.
- Misdiagnosed bipolar patients received inappropriate and costly treatment regimens involving overuse of antidepressants and underuse of potentially effective medications. ... It is recommended that steps be taken to minimize misdiagnosis in clinical settings (Matza LS, et al. 2005).
Nutritional deficiencies
Nutrition plays a key role in every facet of maintaining proper physical and psychological wellbeing. Insufficient or inadeqaute nutrition can have a profound effect on mental health. The emerging field of Nutritional Neuroscience explores the various connections between diet, neurological functioning and mental health.
- Vitamin B6:pyridoxal phosphate (PLP) the active form of B6 is a cofactor in the dopamine serotonin pathway, a deficiency in Vitamin B6 may cause depressive symptoms.
- Folate (vitamin B9) - Vitamin B12 cobalamin : Low plasma and particularly red cell folate and diminished levels of Vitamin B12 have been found in patients with depressive disorders. ...we suggest that oral doses of both folic acid (800 µg/(mcg) daily) and vitamin B12 (1 mg daily) should be tried to improve treatment outcome in depression (Coppen A, Bolander-Gouaille C. 2005)
- Long chain fatty acids: higher levels of omega-6 and lower levels of omega-3 fatty acids has been associated with depression and behavioral change.
Sleep disorders
- Insomnia: the inability to fall asleep is often a symptom of depression, it can also serve in some instances as the trigger for developing a depressive disorder.
- Restless legs syndrome:(RLS), also known as Wittmaack-Ekbom's syndrome, is characterized by an irresistible urge to move one's body to stop uncomfortable or odd sensations. It most commonly affects the legs, but can also affect the arms or torso, and even phantom limbs. Restless Leg syndrome has been associated with Major Depressive disorder. Adjusted odds ratio for diagnosis of major depressive disorder... suggested a strong association between restless legs syndrome and major depressive disorder and/or panic disorder (Lee HB et al. 2008)
- Sleep apnea is a sleep disorder characterized by pauses in breathing during sleep. Each episode, called an apnea, lasts long enough for one or more breaths to be missed, such episodes occur repeatedly throughout the sleep cycle. Undiagnosed sleep apnea may cause or contribute to the severity of depression.
See also
External links
- Strategies for Reducing the Misdiagnosis of Bipolar Depression-Charles M. Bowden M.D.
- Late-Stage Neuropsychiatric Lyme Borelliosis Differential Diagnosis and Treatment
Bibliography
A Dose of Sanity: Mind, Medicine, and Misdiagnosis by Sydney Walker Publisher: Wiley (1997) Language: English ISBN 0471192627
References
- Neuroimaging: a new training issue in psychiatry? -- Bhriain et al. 2005 -
- College Students Exhibiting More Severe Mental Illness, Study Finds
- Grace GD, Christensen RC. Prim Care Companion J Clin Psychiatry. 2007;9(6):433-6.PMID 18185822
- Physical illness presenting as psychiatric disease. Hall RC et al. Arch Gen Psychiatry. 1978 Nov;35(11):1315-20. PMID 568461
- Hall RC, Gardner ER, Stickney SK, LeCann AF, Popkin MK (1980). "Physical illness manifesting as psychiatric disease. II. Analysis of a state hospital inpatient population". Archives of General Psychiatry. 37 (9): 989–95. PMID 7416911.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - Is It Depression--or a Tumor? - Newsweek Nov 21, 2007
- Bushara KO. Neurologic presentation of celiac disease. Gastroenterology. 2005 Apr;128(4 Suppl 1):S92-7. PMID 15825133
- James, William; Berger, Timothy; Elston, Dirk (2005). Andrews' Diseases of the Skin: Clinical Dermatology. (10th ed.). Saunders. ISBN 0-7216-2921-0.
- Lupus Disease Activity May Cause, Worsen Depression — Psychiatric Newsby J Arehart-Trechel - 2006
- Fallon BA, Nields JA. Lyme disease: a neuropsychiatric illness. Am J Psychiatry. 1994 Nov;151(11):1571-83.PMID 7943444
- Friedrich F. et al. Manifest psychosis in neurosyphilis. Gen Hosp Psychiatry. 2009 Jul-Aug;31(4):379-81. Epub 2008 Oct 9. PMID 19555800
- García HH, Evans CA, Nash TE; et al. (2002). "Current consensus guidelines for treatment of neurocysticercosis". Clin. Microbiol. Rev. 15 (4): 747–56. doi:10.1128/CMR.15.4.747-756.2002. PMC 126865. PMID 12364377.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - Sorvillo FJ, DeGiorgio C, Waterman SH. Deaths from cysticercosis, United States. Emerg Infect Dis. 2007 Feb;13(2):230-5.PMID 17479884
- de Almeida SM, Gurjão SA. Frequency of depression among patients with neurocysticercosis. Arq Neuropsiquiatr. 2010 Feb;68(1):76-80. PMID 20339658
- Carruthers VB, Suzuki Y. Effects of Toxoplasma gondii infection on the brain. Schizophr Bull. 2007 May;33(3):745-51. Epub 2007 Feb 23.PMID 17322557
- Henriquez SA, et al. Neuropsychiatric disease and Toxoplasma gondii infection. Neuroimmunomodulation. 2009;16(2):122-33. Epub 2009 Feb 11. PMID 19212132
- Nilamadhab Karl, Baikunthanath Misra (2004). . BMC Psychiatry. 4 (1). doi:10.1186/1471-244X-4-1.. PMC 356918.
{{cite journal}}: Check|doi=value (help); Check|url=value (help); Unknown parameter|month=ignored (help) - Murray KO, Resnick M, Miller V. Depression after infection with West Nile virus. Emerg Infect Dis . 2007 Mar . Available from
- MedicineNet.com Definition of Anemia
- Onder G et al.Anemia is associated with depression in older adults: results from the InCHIANTI study. J Gerontol A Biol Sci Med Sci. 2005 Sep;60(9):1168-72.PMID 16183958
- CDC - Chronic Fatigue Syndrome Jul 1, 2010 ... CDC Centers for Disease Control and Prevention Chronic Fatigue Syndrome.
- Griffith JP, Zarrouf FA. A Systematic Review of Chronic Fatigue Syndrome: Don't Assume It's Depression. Prim Care Companion J Clin Psychiatry. 2008;10(2):120-8. PMID 18458765
- MacHale SM. et al. Cerebral perfusion in chronic fatigue syndrome and depression. Br J Psychiatry. 2000 Jun;176:550-6. PMID 10974961
- Carbohydrate malabsorption syndromes and early signs of mental depression in females. Ledochowski M, et al. Dig Dis Sci. 2000 Jul;45(7):1255-9. PMID 10961700
- Fructose malabsorption is associated with early signs of mental depression. Ledochowski M, et al. Eur J Med Res. 1998 Jun 17;3(6):295-8. PMID 9620891
- Ledochowski M, et al. Fructose- and sorbitol-reduced diet improves mood and gastrointestinal disturbances in fructose malabsorbers. Scand J Gastroenterol. 2000 Oct;35(10):1048-52. PMID 11099057
- Musselman DL, Nemeroff CB. Depression and endocrine disorders: focus on the thyroid and adrenal system. Br J Psychiatry Suppl. 1996 Jun;(30):123-8.PMID 8864158
- Iwata M et al. (Article in Japanese, Abstract in English)Seishin Shinkeigaku Zasshi. 2004;106(9):1110-6.PMID 15580869
- McLachlan SM et al. The link between Graves' disease and Hashimoto's thyroiditis: a role for regulatory T cells.Endocrinology. 2007 Dec;148(12):5724-33. Epub 2007 Sep 6. PMID 17823263
- Bohrer T, Krannich Depression as a manifestation of latent chronic hypoparathyroidism. JH.World J Biol Psychiatry. 2007;8(1):56-9.PMID 17366354
- Pituitary Macroadenomas eMedicine
- Meyers CA. Neurobehavioral functioning of adults with pituitary disease. Psychother Psychosom. 1998;67(3):168-72. PMID 9667064
- Ezzat S. et al. The prevalence of pituitary adenomas: a systematic review. Cancer. 2004 Aug 1;101(3):613-9. PMID 15274075
- Alicja Furgal-Borzycha; et al. (2007). "Increased Incidence of Pituitary Microadenomas in Suicide Victims". Neuropsychobiology. 54: 163–166. doi:10.1159/000106475.
{{cite journal}}: Cite has empty unknown parameter:|urlview=(help); Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help) - Forensic Neuropathology p. 137 By Jan E. Leestma
- Weitzner MA, Kanfer S, Booth-Jones M.J Apathy and pituitary disease: it has nothing to do with depression. Neuropsychiatry Clin Neurosci. 2005 Spring;17(2):159-66. PMID 15939968
- Dowdy DW. et al. Intensive care unit hypoglycemia predicts depression during early recovery from acute lung injury.Crit Care Med. 2008 Oct;36(10):2726-33. PMID 18766087
- Is It Depression--or a Tumor? - Newsweek Nov 21, 2007
- Lahmeyer HW. Frontal lobe meningioma and depression. J Clin Psychiatry. 1982 Jun;43(6):254-5. PMID 7085582
- Rao V, Lyketsos C (2000). "Neuropsychiatric sequelae of traumatic brain injury". Psychosomatics. 41 (2): 95–103. doi:10.1176/appi.psy.41.2.95. PMID 10749946.
- McHugh T, Laforce R, Gallagher P, Quinn S, Diggle P, Buchanan L (2006). "Natural history of the long-term cognitive, affective, and physical sequelae of mild traumatic brain injury". Brain and Cognition. 60 (2): 209–211. PMID 16646125.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Legome E. 2006. Postconcussive syndrome. eMedicine.com. Accessed January 1, 2007.
- Schnadower D, Vazquez H, Lee J, Dayan P, Roskind CG (2007). "Controversies in the evaluation and management of minor blunt head trauma in children". Current Opinion in Pediatrics. 19 (3): 258–264. doi:10.1097/MOP.0b013e3281084e85. PMID 17505183.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Bigler ED (2008). "Neuropsychology and clinical neuroscience of persistent post-concussive syndrome". Journal of the International Neuropsychological Society. 14 (1): 1–22. doi:10.1017/S135561770808017X. PMID 18078527.
- Evans RW (2004). "Post-traumatic headaches". Neurological Clinics. 22 (1): 237–249. doi:10.1016/S0733-8619(03)00097-5. PMID 15062537.
- Iverson GL. Misdiagnosis of the persistent postconcussion syndrome in patients with depression. Arch Clin Neuropsychol. 2006 May;21(4):303-10. Epub 2006 Jun 23. PMID 16797916
- Archiniegas DB, Lauterbach EC, Anderson KE, Chow TW; et al. (2005). "The differential diagnosis of psuedobulbar affect (PBA). Distinguishing PBA among disorders of mood and affect. Proceedings of a roundtable meeting". CNS Spectr. 10 (5): 1–16. PMID 15962457.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - Moore SR, Gresham LS, Bromberg MB, Kasarkis EJ, Smith RA (1997). "A self report measure of affective lability". J Neurol Neurosurg Psychiatry. 63 (1): 89–93. doi:10.1136/jnnp.63.1.89. PMC 2169647. PMID 9221973.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - Smoking Linked to Increased Depression Risk / Medscape
- Hemenway D, Solnick SJ, Colditz GA. Smoking and suicide among nurses. Am J Public Health. 1993 Feb;83(2):249-51. PMID 8427332
- Thomas Bronischa, Michael Höflerab, Roselind Liebac (2008). "Smoking predicts suicidality: Findings from a prospective community study". Journal of Affective Disorders. 108: 135–145. doi:10.1016/j.jad.2007.10.010.
{{cite journal}}: Unknown parameter|issues=ignored (help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - Miller M, Hemenway D, Bell NS, Yore MM, Amoroso P. Cigarette smoking and suicide: a prospective study of 300,000 male active-duty Army soldiers JAm J Epidemiol. 2000 Jun 1;151(11):1060-3. PMID 10873129
- Breslau N, Schultz LR, Johnson EO, Peterson EL, Davis GC. Smoking and the risk of suicidal behavior: a prospective study of a community sample. Arch Gen Psychiatry. 2005 Mar;62(3):328-34. PMID 15753246
- Murphy JM et al. Cigarette smoking in relation to depression: historical trends from the Stirling County Study.Am J Psychiatry. 2003 Sep;160(9):1663-9.PMID 12944343
- Lembke A et al. Depression and smoking cessation: Does the evidence support psychiatric practice? Neuropsychiatr Dis Treat. 2007 August; 3(4): 487–493. PMCID: PMC2655079
- Aronson KR. et al. Smoking is associated with worse mood on stressful days: results from a national diary study. Ann Behav Med. 2008 Dec;36(3):259-69. Epub 2008 Dec 6. PMID 19067100
- A Study of Antihypertensive Drugs and Depressive Symptoms (SADD-Sx)... Ried LD et al. Psychosom Med. 2005 May-Jun;67(3):398-406. PMID 15911902
- Patten SB, Love EJ. Can drugs cause depression? A review of the evidence. J Psychiatry Neurosci. 1993 May;18(3):92-102. PMID 8499431
- The neurobiology of retinoic acid in affective disorders.Bremner JD, McCaffery P. Prog Neuropsychopharmacol Biol Psychiatry. 2008 Feb 15;32(2):315-31. Epub 2007 Jul 10. PMID 17707566
- Alpha-interferon and mental disorders Debien C et al. Encephale. 2001 Jul-Aug;27(4):308-17. (Article in French, extensive abstract in English) PMID 11686052
- Strategies to reduce misdiagnosis of bipolar depression. Bowden CL. Psychiatr Serv. 2001 Jan;52(1):51-5. PMID 11141528
- Misdiagnosed patients with bipolar disorder: comorbidities, treatment patterns, and direct treatment costs. Matza LS at al. J Clin Psychiatry. 2005 Nov;66(11):1432-40. PMID 16420081
- Hvas AM, Juul S, Bech P, Nexø E.Vitamin B6 level is associated with symptoms of depression. Psychother Psychosom. 2004 Nov-Dec;73(6):340-3. PMID 15479988
- Coppen A, Bolander-Gouaille C. Treatment of depression: time to consider folic acid and vitamin B12. J Psychopharmacol. 2005 Jan;19(1):59-65. PMID 15671130
- Rao NP. et al. Role of vitamin B12 in depressive disorder--a case report. Gen Hosp Psychiatry. 2008 Mar-Apr;30(2):185-6.PMID 18291301
- "Study Links Brain Fatty Acid Levels To Depression". ScienceDaily. Bethesda, MD: American Society For Biochemistry And Molecular Biology. 2005-05-25. Retrieved 2008-01-18.
- Kiecolt-Glaser JK.; et al. (2007). "Depressive symptoms, omega-6:omega-3 fatty acids, and inflammation in older adults". Psychosom Med. 69 (3): 217–204. PMC 2856352. PMID 17401057.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help) - Dinan T. et al. Investigating the inflammatory phenotype of major depression: focus on cytokines and polyunsaturated fatty acids. J Psychiatr Res. 2009 Jan;43(4):471-6. PMID 18640689
- Lustberg L, Reynolds CF. Depression and insomnia: questions of cause and effect. Sleep Med Rev. 2000 Jun;4(3):253-262.PMID 12531168
- Skidmore FM, Drago V, Foster PS, Heilman KM. (2009). Bilateral restless legs affecting a phantom limb, treated with dopamine agonists. J Neurol Neurosurg Psychiatry. 80(5):569-70. doi:10.1136/jnnp.2008.152652 PMID 19372293
- Lee HB et al. Restless legs syndrome is associated with DSM-IV major depressive disorder and panic disorder in the community.J Neuropsychiatry Clin Neurosci. 2008 Winter;20(1):101-5. PMID 18305292
- Harris M. et al. Obstructive sleep apnea and depression. Sleep Med Rev. 2009 Dec;13(6):437-44. Epub 2009 Jul 10. PMID 19596599